There are many types of car accident injuries that people experience during traffic accidents. These can include injuries affecting internal organs and neck, shoulder, and back injuries that might not be immediately apparent.
In addition, arm and leg injuries are commonly reported in car collisions due to their sitting posture and their structural vulnerability during mid-to-high-speed impacts. These injuries can be particularly debilitating, affecting mobility and quality of life.
Additionally, chest injuries from impact with the steering wheel or seatbelt are prevalent, which can lead to broken ribs and other forms of internal damage.
These injuries underscore the complex dynamics of car accidents and their profound impact on the human body. Each injury type, from muscular, ligament, nerve, and soft tissue damage to spinal cord and brain trauma, presents unique challenges in both medical treatment and legal considerations.
What This Article Covers:
- We look at why car accidents result in such a wide variety of injuries.
- We examine the types and range of injuries sustained in car accidents from the least to the most traumatic.
- We identify the types of medical professionals who treat different kinds of car accident injuries.
- We describe the diagnostic tools medical professionals use, such as MRI, CT Scans, and X-rays.
- We describe the parts of our physical anatomy affected by car accidents.
- The mechanics of physical forces on occupants in car accidents.
- The misconceptions people have about car accident injuries.
Why Car Accidents Result in So Many Different Types of Injuries
Car accidents can result in a wide variety of injuries for the following reasons:
Sudden deceleration forces:
When a vehicle collides with another, the sudden deceleration can inflict immense force on the occupants’ bodies.
Physical dynamics of car crashes:
The physical dynamics of a car accident can result in unpredictable variables, such as the angle of impact, the vehicle speed at impact, and the specific point of collision.
These variable factors determine which parts of the body absorb the most significant forces.
Diversity in body type and physical condition of the occupant:
Age, physical condition, and preexisting medical conditions can influence an individual’s vulnerability to certain injuries. In other words, a minor injury for one person could be a serious, life-threatening event for another.
Use of safety features:
Vehicle safety equipment, such as seatbelts and airbags, has been engineered to lessen the severity of injuries. However, for these safety features to be effective, they must be properly used and maintained.
Most Common Types of Injuries in Accident Cases:
- Soft Tissue Injuries
- Cervical Strain (whiplash)
- Bulging and Herniated Disc Injuries
- Spinal Cord Compression Injuries
- Broken Bones – Fractures
- Head and Brain Injuries
- Burn Injuries
- Post-Traumatic Stress Syndrome (PTSD)
Soft Tissue Injuries – Cervical Strain
Whiplash is a trauma-inducing injury involving the cervical spine’s soft tissue and ligaments of the neck and shoulder region. It is caused by the neck being suddenly and forcibly thrown forward and then back again, resembling a whipping motion.
The injury to the tissue and ligaments results from the sudden acceleration and deceleration typical in most rear-end collisions, especially when the rear-ending vehicle travels at a high rate of speed and collides with the car at a complete stop.
Even when the rear-ending vehicle is traveling at speeds between 20 to 35 MPH, which is considered slow-to-moderate, the occupant of the rear-ended vehicle can suffer severe tearing of the soft tissue and ligaments surrounding the cervical spine.
The extent of soft tissue trauma is dependent on age, preexisting conditions, and the physical posture of the driver at impact:
Depending on the age and sitting position of the driver at the moment of impact, the trauma to the neck can result in more severe injuries, such as sustaining a bulging or herniated disc.
An older person with preexisting injuries, such as spinal bone spurs, is especially vulnerable to these forms of disc injuries, which can, in some cases, lead to the need for surgery.
The most common symptoms of whiplash may include:
- Decreased range of motion of the neck
- The presence of muscle spasms in the neck and back
- Neck, shoulder, and back pain
- Cervical and thoracic swelling
Wellness Tip
Chiropractic Treatment
Chiropractors
Chiropractors focus on relieving neck and shoulder pain and other whiplash effects, which can become chronic if not treated early.
Chiropractic treatments can include spinal adjustments, which may reduce symptoms by decreasing pain, muscle spasms, and tissue inflammation.
Chiropractic treatment can also help restore the full range of cervical movement after an accident.
Standard therapies chiropractors use include:
- Ice and heat therapies
- Massage
- Spinal Adjustment
- Stretching exercises
- Nutritional advice
- Electrical muscle stimulation
Duration of chiropractic treatment
As with any injury, several factors will influence the duration of chiropractic treatment:
- Severity of damage to tissue and ligaments
- Length of time between injury and treatment
- How well the patient adheres to the treatment plan
- The size and strength of the cervical tissue
- The age and general health of the patient
- Presence of any preexisting condition affecting mobility
Most healthcare practitioners agree that immediate care following an accident is the most effective way to eliminate pain and prevent residual and chronic problems.
The longer the injured person waits to start treatment, the greater the chance of developing a chronic condition and the more difficult it becomes to treat.
Understanding The Spinal Cord
The spinal cord goes from the base of the brain, known as the Medulla, down into the brain stem and through the spinal canal, which comprises protective bone and discs.
At each level, the cord fans out laterally in both directions through openings in the spinal skeletal structure surrounding and protecting the spinal cord.
The spinal cord branches into groups of nerves called nerve roots, which eventually turn into a vast microscopic network of nerves traveling throughout the body.
The four general spine levels from top to bottom
Each spine level contains sublevels separated by discs
- Cervical Spine
- Thoracic Spine
- Lumbar Spine
- Sacral Spine
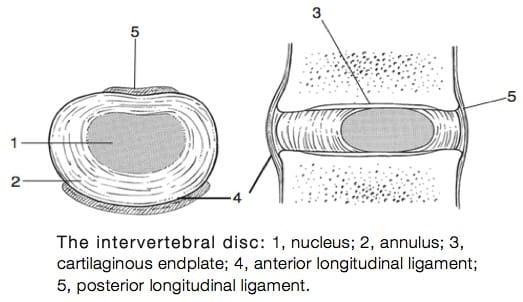
What Is a Disc?
The discs protect the spinal cord and the bone structures of the spinal canal. They comprise about 30% of the spine’s total length.
According to Physiopdia, we have 25 discs that are located in the following regions of our spine:
- Seven discs in the cervical spine
- Twelve discs in the thoracic spine
- Five discs in the lumbar spine
- One disc in the sacral spine
Each disc is a type of circular cushion that functions like a miniature shock absorber between the spine’s protective bone structures of the spinal canal.
Without discs, bones would sit on top of bones and crumble whenever we used our backs to do almost anything, like bending and lifting.
Disc bulges and herniation
When a neck or back is subject to trauma, discs can bulge or herniate into the spinal canal, causing the cord’s nerve roots to be compressed against the bony structures that surround it.
Should the disc press upon the nerve roots that fan out from the spine, it can lead to significant nerve root damage, which can cause shooting pain and loss of sensation.
In severe trauma, the bulging or herniated disc can sometimes compress against the cord’s nerve roots and even the spinal cord itself.
Should part of the spinal cord get compressed, a condition known as myelopathy, it can present a high risk of severe and permanent paralysis of the arms and legs.
Primary causes of herniated discs
Car accidents and heavy falls affecting the back are the most common causes of disc injuries. Herniated disc injuries can be life-changing injuries.
Levels of severity in disc damage:
- Bulging discs
- Ruptured discs
- Fully herniated discs
Diagnosing A Disc Injury and Its Implications
The nature and extent of damage caused by disc bulges or ruptures can be measured by the severity of the physical symptoms they cause in a patient.
In moderate to severe cases, the damage can cause a loss of sensation, strength, and function in our extremities, which can be detected by physical exam and nerve conduction study.
Magnetic resonance imaging (MRI)
The MRI provides three-dimensional, high-contrast images of the spinal cord and surrounding structures.
Suppose an MRI scan reveals disc impingement of a nerve root, which branches out from the spinal canal. In that case, the patient’s symptoms usually manifest as shooting pain, numbness, and stabbing sensations down the arms and legs.
The MRI is often followed by a nerve conduction study (EMG), which measures nerve signal loss from specific nerve groups branching out from the cord.
Nerve damage diagnostics (EMG)
Neurologists, among many other skills, are the physicians who conduct and analyze the results of nerve conduction studies.
The nerve conduction study measures the speed at which electrical signals travel down nerve pathways that activate muscle movement. Ultimately, specific nerve groups can be traced back to nerve roots and associated with a particular level and location of the spine.
Treatment of Minor Disc Injuries
The treatment for minor disk injuries, such as a bulge without herniation, begins conservatively with physical therapy and anti-inflammatories.
The goal of anti-inflammatories is to reduce the swelling near the affected nerve roots so that surgery is not necessary.
Should the pain and numbness continue or worsen, depending on the severity of the symptoms, the patient may have to undergo a discectomy, which is the surgical removal of the bulging or ruptured disc.
The microdiscectomy
Disc injury surgical procedures are much less invasive today. Discs can now be removed through a process known as a microdiscectomy.
Next, we will look at traumatic head injuries, the differences between open and closed-head injuries, and their effects on the brain.
Head And Brain Injury Cases
Traumatic brain injuries (TBI)
Moderate-to-high-speed traffic accidents are a leading cause of traumatic brain injuries. They can range from mild concussions to severe, life-threatening injuries.
Symptoms may include confusion, memory loss, difficulty concentrating, and changes in mood or behavior.
Traumatic brain injury is a critical concern and one of the more severe types of car accident injuries encountered. Such injuries can lead to significant, long-lasting effects and require specialized medical intervention.
Similarly, neck injuries from the whiplash effect during car crashes highlight the unpredictable nature of vehicular accidents.
Neurosurgeons
Serious personal injury accidents sometimes involve head injuries. When this happens, if severe enough, a neurosurgeon should be called into the case to evaluate the patient and, if necessary, be prepared to perform brain surgery.
Neurosurgery has one of the most extended training periods of any medical specialty. Neurosurgical specialists can diagnose and surgically treat damage to the brain and trauma caused to the spinal cord.
Types of Head Injuries
Two major types of head injury
In serious traffic accidents involving head injuries, there are two major types: open and closed head injuries:
Open head injury
Open head injuries penetrate the skull and brain. In these types of head injuries, such as a high-speed head-on car collision in which a metal object penetrates the scalp and brain, the resulting brain dysfunction will be closely correlated to the damaged area of the brain.
An open-head brain injury is often fatal or results in severe and substantial loss of cognitive function and life-long paralysis.
Closed head injury
A closed head injury results from a slip and fall or from a car accident, where the head is bluntly impacted.
These types of impact injuries can have severe consequences, especially if the trauma causes brain swelling, known medically as a subdural hematoma, which usually requires immediate brain surgery to drain the fluid and reduce the swelling.
Loss of consciousness – concussion and blackout
Suppose you have experienced a closed head injury resulting in a loss of consciousness. After a head injury, you should immediately seek medical care if you suffer from one or more symptoms.
The following are possible signs that you suffered a brain injury:
- Memory loss
- Headaches
- Vision loss
- Speech loss
- Fatigue
- Inability to concentrate
- Personality changes
Diagnosing a brain injury
To determine whether you have suffered a brain injury and the extent of neurological damage sustained, you usually need to undergo an MRI scan and neuropsychological testing by an experienced neurologist.
Broken Bones in Traffic Accident Cases
From a legal perspective, broken bones are viewed as a serious personal injury, primarily because of the severe pain and resulting physical limitations they cause.
In the case of multiple broken bones in which surgery has been performed, an extensive rehabilitative period is required for post-surgical physical therapy and recovery, which sometimes can take up to three to four months to complete.
Bone fractures can occur in high and moderate-speed collisions
According to the Centers for Disease Control, in 2018, it was reported that an average of 3.4 million emergency department visits resulted from motor vehicle accident injuries.
Compound and simple bone fractures are car accident victims’ most common orthopedic injuries.
As mentioned, a severe bone fracture could render a person physically incapacitated for months. It can also cause permanent damage to the bones and joints affected.
While high-impact speed impacts are known to cause the most damage to bones and surrounding structures, there are also ways for a person to suffer serious injury from low-to-moderate speed collisions.
For example, consider the case of a stopped driver who hears the sound of screeching breaks behind them.
A common reaction is to brace for impact by locking the arms straight while tightly holding on to the steering wheel. A stiff bracing of the limbs is a common cause of breaks and injury to the arms and wrists and can happen at relatively low-to-moderate speeds.
The need for medical diagnosis and treatment of broken bones
Medically diagnosing a bone fracture and its severity can require a CT Scan or MRI.
Simple radiographs can provide reasonably good views, but certain subtle fractures are not easily detectable through X-rays.
The types of medical treatment usually prescribed for simple bone fractures include positioning the area of the bone break in a cast or soft brace, sometimes traction, followed by physical therapy and home exercises to build muscle and ligament strength.
These remedies do not necessarily include surgery. However, other ways of treating broken bones do require surgery.
The medical specialists who diagnose and treat these injuries include orthopedic physicians, orthopedic surgeons, physical and rehabilitative physicians, and physical therapists.
Surgery For Broken Bones – Open Reduction and Fixation
According to a February 8, 2024, article published by MedlinePlus, the three primary treatment options for bone fractures are:
- Casting
- Open reduction and internal fixation: This involves surgery to repair the fracture. It frequently consists of the insertion of metal rods, screws, or plates to repair the bone so it remains in place under the skin after the surgery. This procedure is used for complicated fractures that cannot be realigned by casting or in cases in which the long-term use of a cast is undesirable.
- Open reduction and external fixation. This type of surgery repairs the fracture and involves placing an external fixation device on the limb with the fracture. The device is an external frame that helps support the bone and holds it in the correct position while it heals.
Injuries To The Shoulder – Impingent Syndrome – Rotator Cuff
Bracing the arm can also do severe shoulder damage to the muscles and tendons of the rotator cuff, causing a painful tearing condition known as impingement syndrome.
Specifically, if the driver’s arm is locked and braced on the steering wheel, the sudden force of a rear-end collision could travel through the arm and into the shoulder, causing severe inflammation of the rotator cuff and even a rotator cuff tear.
Such forces can also cause what is called impingement syndrome of the shoulder. Impingement occurs when the tendons in the shoulder are swollen, pinching, or impinging on the tendons and other structures, causing chronic pain and reduced mobility.
Twisting position of the body upon impact – femur, pelvis, and ribs
One can also suffer a severe injury if the person is in a twisted position immediately before impact and thrown forward and back, as is common in rear-end collisions. The bones most likely to fracture in a moderate-to-high-speed car collision include the femur, pelvis, and ribs.
Legal Tip
Types of Bone Fractures
Many bone fractures include partial or complete fractures, open or closed wound fractures, and stable or displaced fractures. Other common types include:
- Comminuted Fracture (Three or more pieces of the bone are fractured)
- Compression Fracture (A large part of the bone is crushed)
- Depressed Fracture (A fractured bone is pressed inward, such as in a skull fracture)
- Incomplete Fracture (Where only one side of the bone breaks)
The next area of traumatic injuries we will cover is burn injuries. The most serious of them happens in car accidents where a vehicle and its occupants are engulfed in flames and suffer third-degree burns.
Burn Injuries
The occurrence of burn injuries is more common than you might first suspect. According to a March 2020 article from NFPA.org:
- An estimated 212,500 vehicle fires caused 560 deaths and over 1,500 burn injuries in the US during 2018.
- Vehicle fires caused 4.5 times as many deaths as nonresidential structure fires and 1.6 times the number of apartment fire deaths.
- Traffic collisions were the leading cause of vehicle fires that resulted in death.
Three Classifications of Burns
According to the Mayo Clinic, there are three classifications of burns:
First-degree burns
Minor burns only affect the skin’s outer layer and may cause redness, swelling, and pain. It usually heals with first-aid measures within several days to a week. Sunburn is a classic example.
Second-degree burns
This type of burn affects the skin’s outer and secondary skin layers. It usually manifests as red, white, or splotchy skin, is extremely painful, and can cause significant swelling.
Second-degree burns can appear wet before developing into painful blisters. Second-degree burns can cause permanent scarring.
Third-degree burns
Third-degree burns reach below the two skin layers and penetrate the fat beneath the skin, causing wounds to appear charred and black or white. The skin can also appear waxy or leathery.
Third-degree burns destroy nerves and can cause difficulty in breathing. Depending on the extent of third-degree burns, they can be fatal. If not, third-degree burns are life-changing, cause severe deformities, and often require long-term medical care.
Critical Burns – Emergency Management Video:
Post-Traumatic Stress Syndrome
Post-Traumatic Syndrome (PTSD) is more commonly seen in times of war where there are intense and violent exchanges between combatants.
In personal injury cases, PTSD results from a person experiencing a perceived life-threatening injury, such as being in a severe traffic accident. Psychologists and Psychiatrists have seen progress in using cognitive behavioral therapy to treat certain forms of PTSD.
Causes of post-traumatic stress
When danger is perceived, the body is hardwired to trigger an assortment of chemical and hormonal reactions – we are suddenly in immediate fear and apprehension of danger.
We are in an excited state of fight or flight. It is common for people who have PTSD to feel stressed or frightened, even when the threat is no longer present.
PTSD is an anxiety-induced emotional disorder due to exposure to a highly dangerous or life-threatening event. This is commonly seen in severe automobile and traffic accidents where the threat of death or significant bodily injury is perceived as both real and imminent.
Obsessive flashbacks
The most common symptom is the persistent re-experiencing of the traffic accident through obsessive thoughts and flashback memories redundantly being played out over and over again.
It is not uncommon for victims of repeated domestic violence to experience uncontrollable flashbacks and spiraling thoughts about the violence they experienced.
Common symptoms of PTSD
- Feeling easily agitated by noises
- Sleep disorders
- Severe avoidance of locations or events that trigger memories of the trauma
- Loss of control of emotional and individual autonomy
- Experiencing deep feelings of guilt, anxiety and depression
PTSD Treatment Options
When seeking treatment for post-traumatic stress disorder, you will want to consider a healthcare specialist specializing in the treatment of trauma and PTSD.
Beyond the doctor’s credentials and experience in trauma, it’s also vital that the patient feels safe and comfortable with the doctor.
Behavioral and talk therapy
Behavioral therapy slowly reintroduces the patient to their fears and gradually helps them take small steps to overcome them.
Talk therapy can also be quite valuable in this context.
Legal considerations in claiming PTSD
Accident victims rely on their personal injury lawyers to determine whether it makes strategic sense to actively pursue a client’s post-traumatic stress disorder as one of the elements of the accident victim’s damages.
Some juries have been reluctant to award significant amounts for pain and suffering if it is based on a claim for post-traumatic stress disorder rather than severe physical injuries.
7 Common Misconceptions People Have About Car Accident Injuries:
Misconception #1: Minor accidents don’t cause serious injuries.
Reality: Even low-speed collisions can result in significant injuries that may not be immediately apparent.
Misconception #2: You probably weren’t seriously injured if you didn’t feel pain immediately at the time of the accident.
Reality: Some injuries, such as internal bleeding or traumatic brain injuries, may not produce immediate symptoms, making them easy to overlook. Also, soft tissue injuries to the neck, shoulders, and back can sometimes take days before they cause severe pain and limit the person’s mobility.
Misconception #3: Seatbelts always prevent injuries.
Reality: While seatbelts are highly effective, they do not eliminate the risk of injury, particularly in high-speed or severe crashes.
Misconception #4: Airbags are a substitute for seatbelts.
Reality: Airbags are designed to work with seatbelts to provide optimal protection. They are not a replacement for proper seatbelt use.
Misconception #5: Soft tissue injuries, like sprains, are not serious injuries.
Reality: Soft tissue injuries can be very painful and debilitating and take a long time to heal, especially if not properly treated.
Misconception #6: Once you feel better, the injuries have healed.
Reality: The recovery process from car accident injuries can be complex and long-lasting, with the potential for ongoing complications or chronic pain.
Misconception #7: Psychological trauma is not an actual injury.
Reality: Car accidents can lead to significant emotional and psychological harm, such as post-traumatic stress disorder (PTSD), that requires professional treatment.